Multiple Sclerosis
Aetiology : unknown (genetic and environmental)
Prevalence : 40-60 / 100 000 inhabitants (most common autoimmune disease of the central nervous system : more women than men)
Several clinical forms of MS :
Relapsing-Remitting MS : affects about 85% of MS patients (most common form). The symptoms between two flare-ups disappear entirely, in other words, the lesions are reversible.
Secondary Progressive MS : correspond to the aggravation of relapsing–remitting MS. The lesions between two flare-ups are irreversible. Normally, the disease-modifying agents delay such progression.
Primary Progressive MS : affects approximately 15% of MS patients. The lesions are irreversible from the beginning and worsen with time. Disease-modifying agents are inefficient on this form of MS : it’s an unmet medical need.
Main symptoms :
Treatment for crisis :
Corticoids IV, high doses (such as Methylprednisolone)
Main side effects : diabetes induced by the corticotherapy, osteoporosis, electrolytic imbalance leading to hypertension, metabolic troubles, increase the risk of infection, trouble sleeping
à The main objective in this pathology is to prevent the crisis (diminish their number and gravity with the long term treatment).
Long-term treatment :
Disease modifying treatments : Immunomodulatory therapies
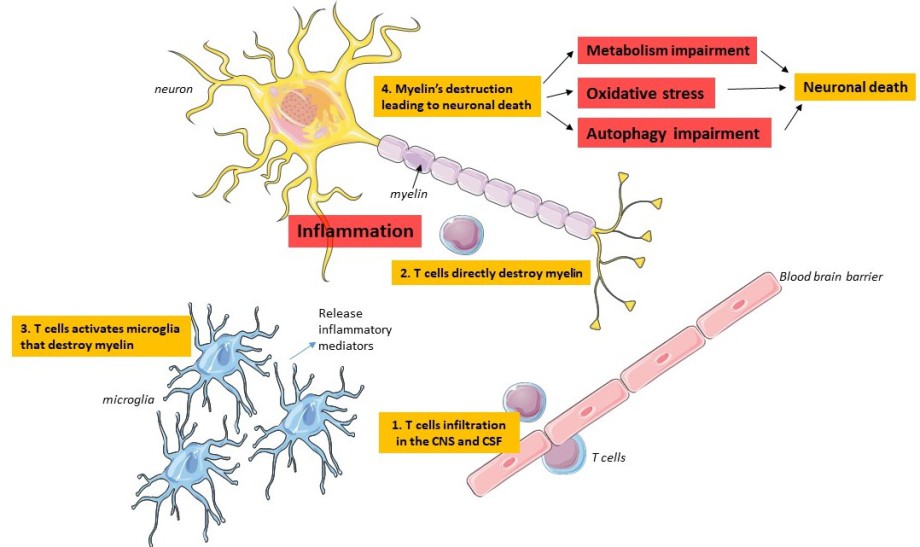
Mainly, they try to stop the overactivation of T cells in the blood but also directly in cortex and lymph nodes.
Problems : only effective in the Relapsing-Remitting MS, most of the treatments are injections (subcutaneous SC, intramuscular IM, intraveinous IV), 1 to 3 times a week or everyday which is very constraining for the patient.